Age-Related Macular Degeneration (AMD)
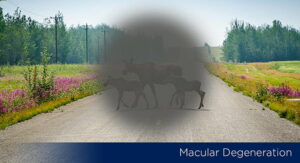
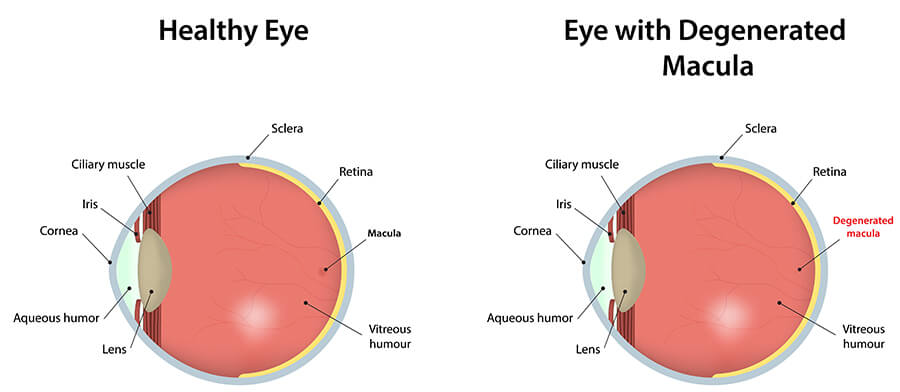
With the aging of our population, age-related macular degeneration (AMD) is a common eye disease our Vitreoretinal Surgeons and Retina Specialist see among Maine seniors at Eyecare Medical Group in Portland. Macular degeneration or age-related macular degeneration (AMD) is a disease of the retina in which the central portion of the retina, called the macula, is damaged. The macula is responsible for providing central vision. Central vision is the sharpest or clearest area of your vision and is required for activities such as seeing fine detail of faces, reading and recognizing colors. Most people do not realize that macular degeneration is an incurable eye disease or that it is the leading cause of legal blindness for those aged 55 and older in the United States. It affects the vision of more than 10 million Americans.
There are a number of different types of degenerative macular diseases. Age-related Macular Degeneration (AMD) is the most common type of macular degeneration. The older you are, the greater the chance that Macular Degeneration will affect you.
Macular Degeneration is a complex eye disease. Fortunately, with early diagnosis, it is possible to have a number of treatment options available to help preserve vision.
Causes of Macular Degeneration (AMD)
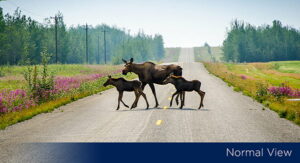
Understanding the causes of age-related macular degeneration (AMD) is an important part of helping seniors preserve their eye health and vision. Age-related macular degeneration is a degenerative condition of the macula that is caused by the hardening of the small arteries supplying oxygen and nutrients to the retina. The hardening and narrowing of these arteries deprive the macula of oxygen and nutrition. This results in a slow but progressive loss of function. The visual effects of macular degeneration can be relatively minimal with a mild “dimming” or “distortion” of your central vision, or they can be quite profound resulting in a complete loss of your central vision. However, macular degeneration DOES NOT cause total blindness. Since the effect of macular degeneration is limited to the central retina, its effects are limited to central vision and thus it does not cause any loss of your peripheral vision.
Macular Degeneration is a complex eye disease. Fortunately, with early diagnosis it is possible to have a number of treatment options available to help preserve your vision.
Wet & Dry Types of Macular Degeneration (AMD)
When patients are diagnosed with age-related macular degeneration (AMD) by the Eyecare Medical Group Vitreoretinal Surgeons and Retina Specialists in Portland, they will most likely be identified as having one of two types of age-related macular degeneration (AMD): Dry Macular Degeneration or Wet Macular Degeneration
Dry Macular Degeneration
Dry Macular Degeneration, also called Atrophic Macular Degeneration, is the most common type of age-related macular degeneration. Dry macular degeneration makes up approximately 85-90% of cases of macular degeneration. If you have dry macular degeneration diagnosed during the examination of your retina, your eye doctor will see small, yellow-colored deposits between the retinal layers, which are called drusen. Dry Macular Degeneration may result in a slow, gradual progressive “dimming” of your central vision.
Many people 50 years of age or older begin to display some drusen as they age. Drusen are not a direct problem for your vision unless they are large or confluent. If you have drusen, your eye doctor may ask you to schedule eye examinations more frequently in order to monitor them, as there is some possibility that dry macular degeneration will progress to wet macular degeneration over a period of time. Thus people with dry macular degeneration, even without any noticeable change in vision, need to be followed closely as wet macular degeneration has far more serious consequences for vision loss.
Wet Macular Degeneration
Wet Macular Degeneration is far more likely to cause serious vision loss than dry macular degeneration. Fortunately, it only accounts for about 10-15% of cases of macular degeneration. Wet macular degeneration is characterized by an abnormal growth of new blood vessels under the retina. These new blood vessels are called “neovascularization”. Neovascularization does not behave like “normal” blood vessels in that the new vessels are unusually weak in their structure. In fact, they are quite fragile and are prone to be leaky and can easily break and bleed. If leakage occurs, the macula may actually begin to swell. If the new blood vessels break and bleeding occurs, it can result in scarring as it heals. Scarring of the macula can cause a sudden, rapid and severe loss of central vision, which is irreversible.
Macular Degeneration is a complex eye disease. Fortunately, with early diagnosis it is possible to have a number of treatment options available to help preserve your vision.
Diagnosis of Macular Degeneration (AMD)
The Vitreoretinal Surgeons and Retina Specialists at Eyecare Medical Group in Portland have extensive experience and expertise in the diagnosis of macular degeneration (AMD). As with most eye conditions and diseases, it is important to have routine eye examinations in order to help preserve eye health and vision. By scheduling regular eye exams, you are giving yourself the advantage of allowing your eye doctor to make an early diagnosis of macular degeneration. More importantly, if at any time you experience any “distortion” or “twisting”, “shadowing” or “bending” of objects in your vision, you should schedule an appointment at Eyecare Medical Group immediately. Be sure to let the receptionist know that you are experiencing these symptoms.
If you are over the age of 40-45 and anyone in your family has been told that they have macular degeneration, it is a good idea to have a complete eye examination each year. Make certain that you tell the eye doctors and staff at Eyecare Medical Group if you have a family history of macular degeneration. During your eye examination, eye drops will be put in your eyes to dilate your pupils in order to carefully examine the macula and retina using various types of instruments and sources of high magnification.
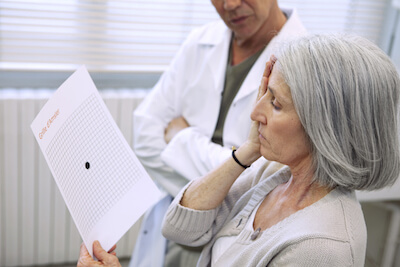
Additional tests that your doctor may perform to further evaluate the macula during your eye examination can include checking your color vision and an Amsler Grid Test, which helps identify distortion of your central vision and may be an indication of swelling or fluid under the Macula.
Amsler Grid
While it may appear simple, the Amsler Grid Test is actually a very significant test. By using the Amsler Grid, it is possible to detect small changes in your vision that can result from the accumulation of just a small amount of fluid under your Macula. Your eye doctor may actually recommend that you take an Amsler Grid home and use it each day to check for slight changes in your vision. If this is necessary, your eye doctor and staff will supply you with an Amsler Grid and detailed instructions on how to use it.
If your doctor detects any signs of macular degeneration or he or she believes that you may be at risk for macular degeneration, they will schedule an appointment for you with an Eyecare Medical Group Retina Specialist as additional testing may be necessary. Our Retina Specialists may find it necessary for you to have some specialized color pictures and testing taken of the macula and retina. The two most common tests are Intravenous Fluorescein Angiogram (IVF) and Optical Coherence Tomography (OCT). During an IVF a special fluorescent dye is injected into a vein in your arm. By using a high-speed digital camera, a series of photographs will be taken in rapid succession as the dye passes throughout the retinal blood vessels. From these pictures, if present, your Retina Specialist will be able to see any fluid leakage or new blood vessel growth beneath the retina. An OCT test does not require any injections. It uses light waves in a fashion similar to ultrasound to very precisely measure your retina. Your eye doctor will be able to see if you have fluid in your retina, and if so, how much. This test is especially useful to monitor for changes although both the IVF and OCT tests will also show any changes or damage to the macula and retina and the extent of the changes. Most importantly, these tests give us a considerable amount of information regarding whether certain types of treatments such as Laser Treatment for Macular Degeneration or Intravitreal Injections such as Avastin®, Eylea® or Lucentis® might help stabilize your vision and prevent vision loss. Today, thanks to the advances in treating Wet Macular Degeneration, if caught early, it may be possible to avoid significant vision loss.
Macular Degeneration is a complex eye disease. Fortunately, with early diagnosis it is possible to have a number of treatment options available to help preserve your vision.
Treatment of Macular Degeneration (AMD)
The Vitreoretinal Surgeons and Retina Specialists at Eyecare Medical Group in Portland have extensive experience and expertise in the treatment of macular degeneration (AMD). If Macular Degeneration is diagnosed early enough, we are very fortunate to have a number of possible treatment options that may help to slow or even halt the progression of vision loss from Macular Degeneration. However, patients must understand that once the Macula has been damaged, there is no treatment that currently can reverse that damage and the associated loss of vision. Early diagnosis and treatment to prevent or halt vision loss must be the approach that we take.
Macular Laser Photocoagulation
A number of years ago, a distinguished group of eye surgeons and macular disease specialists formed The Macular Photocoagulation Study Group in order to conduct well-controlled international clinical studies to determine what particular macular conditions should be treated with lasers, what types of lasers should be used, which patients might get the best results and to try and establish the best ways to use lasers to treat macular degeneration. The results of these studies suggested that even in cases where a successful laser treatment was performed, leakage returned in 50% of the cases within 2 years. The overall guidelines for Laser Photocoagulation for Macular Degeneration suggest that laser treatment is limited in its effectiveness and may also lead to scarring of the Macula and additional vision loss. Thus we tend to emphasize the use of therapeutic injections of Vascular Endothelial Growth Factor Inhibitors (VEGF) to treat macular degeneration.
Vascular Endothelial Growth Factor Inhibitors (VEGF) Avastin®, Eylea®, and Lucentis® Injections
Resulting from basic research in cancer therapy in the area of “angiogenesis” or new blood vessel growth, a large base of knowledge has been developed in the treatment of Wet Macular Degeneration. Researchers discovered that a specific protein called “Vascular Endothelial Growth Factor” (VEGF) causes the growth of new blood vessels or “neovascularization” to occur in the eye. From this work, drugs can be injected into the eye in order to slow or stop the growth of new blood vessels. Two drugs, Eylea® and Lucentis® have been developed and FDA approved with specific indications to treat Wet Macular Degeneration. Each of these drugs works by inhibiting Vascular Endothelial Growth Factor (VEGF) to limit the stimulus to grow new blood vessels in the Retina.
Eylea® and Lucentis® Injections are intravitreal injections-that means an injection that is placed directly into the Vitreous of the eye. Generally, they need to be repeated every four to six weeks. Clinical studies of these anti-VEGF Injections indicate that when given to patients who have evidence of new blood vessel formation monthly over 90% of patients will maintain their vision.
The anti-VEGF Injection is performed by prescription only and injected only by Eyecare Medical Group Vitreoretinal Surgeons and Retina Specialists.
Should you have or be at risk for Wet Macular Degeneration, they will discuss the testing and treatment results with you. They will also be able to tell you more about the length of your actual treatment program, as it varies for each patient. If Avastin® Injection, Eylea® Injection or Lucentis® Injection is a possible option; we will spend the time necessary to thoroughly review the possible risks, benefits and side effects with you before you decide to proceed.
Age-Related Macular Degeneration & Diet
There are a number of studies that have strongly suggested that nutrition may play a role in the likelihood of developing Macular Degeneration. Simply stated, it appears that people who have a diet that is rich in fruits and vegetables-particularly green leafy vegetables-have a considerably lower incidence of macular degeneration. It is not yet clear whether taking dietary supplements can prevent progression in patients with existing macular disease, but it does seem clear that certain dietary supplements can reduce your risk of macular degeneration. The age-related eye disease Study (AREDS), which was sponsored by the National Eye Institute, showed that taking high levels of antioxidants and Zinc could reduce the risk of developing age-related macular degeneration by about 25%. This is not a cure, but we need to consider this as a possible way to help patients who are at risk for age-related macular degeneration prevent vision loss.
A VERY SPECIFIC FORMULATION WAS USED IN THIS STUDY
BEFORE patients begin taking any course of vitamin or antioxidant supplements, you should fully discuss the risks and benefits with our Retina Specialists, who will determine in consultation with your family physician or Internist if necessary, whether this is safe and effective for you.
Macular Degeneration is a complex eye disease. Fortunately, with early diagnosis, it is possible to have a number of treatment options available to help preserve your vision.
Macular Disease
At Eyecare Medical Group our Retina Specialists examine and treat patients with other types of macular disease besides age-related macular degeneration (AMD). Some other types of macular disease that patients should be familiar with given their ability to significantly affect vision include the formation of a Macular Hole, Macular Pucker or Epi-Retinal Membrane and Central Serous Chorioretinopathy (CSCR).
Macular Hole
At Eyecare Medical Group our Retina Specialists examine and treat patients with a macular hole. A macular hole is a condition that affects the very central portion of the retina.
A macular hole may occur for a number of reasons including eye injuries, inflammation inside the eye and most commonly, the normal aging process. As we age, the vitreous gel in the back of our eye becomes more liquefied and often results in a Vitreous Detachment with associated floaters. Sometimes, when the Vitreous “pulls’ it can actually form a macular hole.
Macular holes often begin slowly but usually will affect central vision depending on the severity. They can occur as partial holes only affect a part of the macular layers, causing wavy, distorted, blurred vision or they can occur as full-thickness holes causing a complete loss of central vision.
Signs and Symptoms of Macular Holes
The severity of the symptoms of Macular Holes depends on whether the hole is a partial thickness or full thickness, but in general, may include the following:
- Blurred Central Vision
- Distorted, “Wavy” Vision
- Difficulty reading or seeing fine detail even with glasses
- Grayish Area in Central Vision
- Central Blind Spot or “Dark Spot”
Diagnosis and Treatment of Macular Holes
Macular Holes are easily detected through visual acuity testing in conjunction with an Amsler Grid Test, a dilated pupil examination of the macula with an Ophthalmoscope and Slit Lamp High Magnification Fundus Lens, Optical Coherence Tomography (OCT) and sometimes an Intravenous Fluorescein Angiogram (IVF) or other specialized photographs.
Some macular holes seal by themselves and do not require treatment. In many cases, however, a surgery called vitrectomy is necessary to close the hole and restore useful vision. During Vitrectomy, the Retinal surgeon will gently remove the Vitreous gel in order to eliminate any traction on the Macula. A gas bubble is then injected into the eye to place gentle pressure on the Macula and help the hole to seal. In many cases, patients enjoy functional vision after the bubble has been absorbed and the eye has healed.
Macular Pucker, Epi-Retinal Membrane, Cellophane Maculopathy & Vitreomacular Adhesion (VMA)
The Retina Specialists at Eyecare Medical Group examine and treat patients with an epiretinal membrane, also referred to as a macular pucker or cellophane maculopathy.
This retinal condition describes a cellophane-like membrane forming over the macula, or the central part of the retina. It is typically a slow-progressing problem that can affect the central vision by causing blur or distortion. As it progresses, the membrane may cause traction and lead to swelling of the macula.
Epiretinal Membrane
Epiretinal membranes (ERMs) are more often seen in people over 70 years of age. Its exact cause is not completely understood, and the majority of ERMs have no associated ocular abnormality. Epiretinal membranes can be associated with other eye problems such as Diabetic Retinopathy, Posterior Vitreous Detachment, Macular Hole, and Retinal Detachment.
Signs and Symptoms of Epiretinal membranes
The signs and symptoms of Epiretinal membranes may include:
- Blurred Vision
- Double Vision in the affected eye
- Distorted Vision – straight lines appear bent or wavy
Diagnosis and Treatment of Epiretinal membranes
Epiretinal membranes are diagnosed with a dilated fundus examination and Optical Coherence Tomography (OCT). If there is a significant effect on vision, a surgical procedure to “peel” the epiretinal membrane may be considered. If there is no or minimal effect on vision, observation is usually recommended.
Central Serous Chorioretinopathy
Central Serous Chorioretinopathy is a retinal disorder that typically affects young to middle-aged patients, more often men. It is characterized by a serous detachment of the retina, or an accumulation of serous fluid underneath the retina, usually in the central macular area. Central Serous Chorioretinopathy is usually self-limiting, and most patients will have spontaneous recovery within a few months without significant visual loss. Some patients may develop chronic or recurrent disease that can lead to visual loss. Up to 50% of patients with Central Serous Chorioretinopathy can develop a recurrence which can happen at any time, but often within the first year after the first episode.
Symptoms of Central Serous Chorioretinopathy
Many patients first notice a minor blurring of vision, followed by varying degrees of “metamorphopsia” or distorted vision, “micropsia” or the perception that objects are smaller than they actually are, “chromatopsia” or objects looking unusually colored, or a shift of prescription toward farsightedness or hyperopia. Visual acuity may range from 20/20 to 20/200 or worse.
Diagnosis and Treatment of Central Serous Chorioretinopathy
Central Serous Chorioretinopathy is diagnosed with a dilated fundus examination along with Optical Coherence Tomography (OCT), Fluorescein Angiography (FA), and possibly Indocyanine Green Angiography (ICG). Although most cases resolve without treatment, laser photocoagulation or photodynamic therapy may be considered in chronic or recurrent cases.





