Diabetic Retinopathy & Eye Problems

Diabetic eye disease and diabetic eye problems, such as diabetic retinopathy, are areas of specialization for the retina specialists and vitreoretinal surgeons at Eyecare Medical Group. Each has extensive experience in diagnosing and treating the retinal complications of diabetes.
There are many patients with diabetes mellitus who think that the underlying disease is simply an inability to effectively metabolize and process glucose. Unfortunately, the reality is that the effects of diabetes are considerably more widespread and actually affect many organs and tissues throughout your body. Diabetes is actually a disease of the small blood vessels throughout the body. When diabetes damages these small blood vessels it will impair the normal circulation of blood in certain organs and tissues. It is quite common for patients with diabetes to experience difficulty with the circulation in their legs, kidneys, heart, brain and eyes-especially the very small blood vessels of the eye found in the retina. When diabetes causes damage to the small blood vessels in the retina, it is called diabetic retinopathy.
According to the Centers for Disease Control, diabetes affects approximately 26 million people in the United States. Recent data from the Prevent Blindness America Vision Problems in the U.S. report confirm that diabetes is the leading cause of new cases of blindness in adults 20-74 years of age. There are almost 8 million people ages 40 and older who have diabetic retinopathy, a complication characterized by a weakening of blood vessels in the retina so that they break down, causing the retina to swell, hemorrhage and become deprived of oxygen and nutrients, ultimately leading to vision loss. This represents an 89 percent increase in incidence between the years 2000-2012. Although there is no cure for diabetic eye disease, annual eye exams for diabetes patients are essential to help slow the progression of the disease. With early diagnosis and treatment, the progression of the disease and its associated vision loss can at a minimum be slowed, and in many cases, vision loss from diabetic retinopathy can be prevented.
Stages of Diabetic Retinopathy
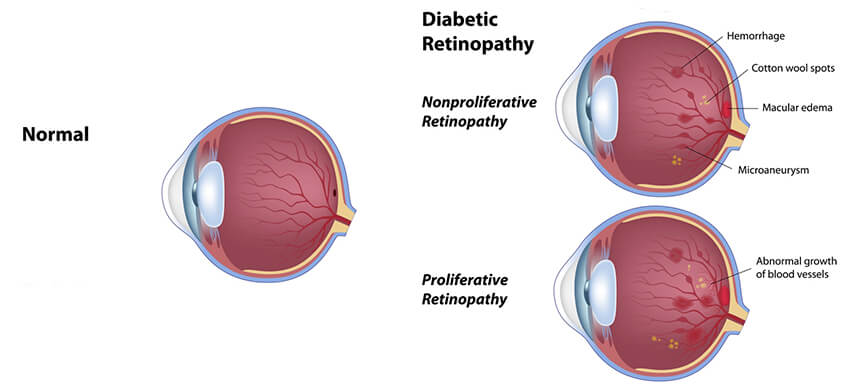
Diabetic retinopathy typically appears and then progresses in stages. These stages include the following:
Mild Nonproliferative Retinopathy
Mild nonproliferative retinopathy is the earliest stage of diabetic retinopathy. It is characterized by the presence of “dot” and “blotch” hemorrhages and “microaneurysms” in the retina during your eye examination. Microaneurysms are areas of balloon-like swelling of the tiny blood vessels in the retina. Early nonproliferative retinopathy can be present without any change in your vision. Nonproliferative retinopathy usually does not require treatment unless it progresses or if it is accompanied by diabetic macular edema. If you have nonproliferative retinopathy, your doctor will make specific recommendations about how often you will need to be reexamined.
Moderate Nonproliferative Retinopathy
Moderate nonproliferative retinopathy is a slightly more severe stage of diabetic retinopathy. During this stage, some of the small blood vessels become increasingly damaged. This damage causes a decrease in the supply of nutrients and oxygen to certain areas of the retina.
The best way to diagnose injury to small blood vessels in the retina is by having a diagnostic test called an Intravenous Fluorescein Angiogram (FA). The intravenous fluorescein angiogram is performed right in our office. We perform the FA by injecting a dye into a vein in your arm and then, using a specialized camera, take a series of photographs of the retina as the dye circulates throughout the retinal blood vessels. Using the FA, it is possible for the Eyecare Medical Group vitreoretinal surgeons and retina specialists to precisely and directly observes the circulation and the integrity of the blood vessels in the retina so that they can identify any blood vessels that may be blocked.
Severe Nonproliferative Retinopathy
Severe nonproliferative retinopathy is the next progression of diabetic retinopathy. Severe nonproliferative retinopathy is characterized by a significant number of small blood vessels in the retina becoming blocked. As a greater number of blood vessels become blocked, it results in more areas of the retina being deprived of nourishment and oxygen. A lack of sufficient oxygen supply to the retina results in a condition called “Retinal Ischemia”.
Proliferative Retinopathy
Proliferative retinopathy is a stage of diabetic retinopathy that carries a significant risk of vision loss. The retina responds to a lack of oxygen, or ischemia, by attempting to compensate for the reduced circulation by growing new, but abnormal blood vessels-a process called neovascularization. When retinal neovascularization is present, you have progressed into the stage of diabetic retinopathy called proliferative retinopathy. Retinal neovascularization includes abnormal blood vessels that are extremely fragile and tend to break easily and bleed into the vitreous. If left untreated, proliferative retinopathy may result in hemorrhaging into the vitreous or lead to scarring and retinal detachment with profound vision loss, even blindness.
It may be possible for patients to have early proliferative retinopathy and retinal neovascularization with good vision. So, even if proliferative retinopathy and retinal neovascularization do not appear to be causing any vision loss, it is critical that it is treated as quickly as possible to stop disease progression.
Diabetic Macular Edema
Diabetic macular edema is a common diabetic eye problem that can cause blurry vision and even vision loss. Normally, the small blood vessels in the retina do not leak. One of the early effects of diabetes is to cause the blood vessels in the retina to begin to leak due to weakening the inner lining of the blood vessels so that they become porous. Leakage from the retinal blood vessels may cause the center of the retina, the macula, to actually swell, a condition called diabetic macular edema. Diabetic macular edema can occur in any stage of diabetic retinopathy.
The diagnosis of diabetic macular edema is an indication that the breakdown of the retinal blood vessels from diabetes is beginning and requires careful monitoring. In the discussion about your stage of diabetic retinopathy, we will make specific recommendations about how often you will need to return for eye examinations and the need for additional photographs, fluorescein angiograms or OCT scans. Please be sure to keep these appointments, as they are critical in helping you maintain your eye health and vision.
Treatment of Diabetic Retinopathy
The Eyecare Medical Group vitreoretinal surgeons and retina specialists are experienced in all types of treatment for diabetic retinopathy. Depending on the stage of diabetic retinopathy, the potential for and the amount of vision loss, it is possible to treat, stabilize and often reverse the effects of the disease. Treatment of diabetic retinopathy can entail the use of retinal laser photocoagulation treatment as well as intravitreal injections of Vascular Endothelial Growth Factor (VEGF) Inhibitor drugs or other drugs. However, successful management of diabetic eye problems requires early diagnosis and treatment.
Treatment of Diabetic Retinopathy
The National Institutes of Health and the National Eye Institute have funded a number of large scale, multi-center, controlled studies that have produced clinical care guidelines for diabetic retinopathy used by our physicians. These include:
We use the results of these studies to guide patients in the treatment of diabetic retinopathy since with early treatment it is possible for patients with diabetic retinopathy to have only half the likelihood of losing vision as compared to those patients who fail to receive early treatment.
Diabetic Laser Treatment
Nonproliferative Retinopathy & Laser Treatment
During the early stages of mild nonproliferative retinopathy, moderate nonproliferative retinopathy and the beginning of severe nonproliferative retinopathy, it is not likely that you will need laser treatment unless you have diabetic macular edema.
Proliferative Retinopathy & Laser Treatment
Proliferative Retinopathy is treated with a Retinal Laser Photocoagulation procedure called “Scatter Laser Treatment” or “Pan Retinal Photocoagulation”. The goal of scatter laser treatment is to shrink abnormal blood vessels. Your doctor will place approximately 1,000 to 2,000 laser spots in areas of the retina away from the macula, causing the abnormal blood vessels to shrink. Since scatter laser treatment requires a large number of laser spots, it is often necessary to use two or more sessions to complete the laser treatment.
Sometimes patients who have had Scatter Laser Photocoagulation will experience some loss of their side or peripheral vision, some loss of night vision and a decrease in color vision. However, scatter laser treatment is necessary to preserve the rest of your vision and stop the progression of the disease. Sometimes Scatter Laser Photocoagulation might be used in combination with intravitreal injections of Vascular Endothelial Growth (VEGF) Inhibitors such as Lucentis®, Avastin® or Eylea® Injections.
When Scatter Laser Treatment with or without Vascular Endothelial Growth (VEGF) Inhibitors is unsuccessful in stopping the progression of the proliferative retinopathy and when a vitreous hemorrhage occurs and does not clear on its own, or when a retinal detachment develops, then a vitrectomy is often helpful. A vitrectomy involves inserting instruments into the eye, and removing the vitreous gel, any blood present in the vitreous cavity, and removing the scar tissue that has grown on the surface of the retina.
Diabetic Macular Edema & Laser Treatment
Diabetic Macular Edema is best treated with one of two types of Retinal Laser Photocoagulation procedures called Focal Laser Treatment and Grid Laser Treatment. Focal Laser treatment is used to close leaking microaneurysms in a limited area and Grid Laser treatment is used to treat a more diffuse swelling in the macula. With either type of Laser Treatment for Macular Edema, your doctor will place laser spots in the areas of retinal leakage surrounding the macula. These spots act to slow the leakage of fluid and reduce the amount of fluid in the retina. It is usually possible to complete these Laser Treatments in one session, however, depending on the results, additional treatment may be necessary. You may need to have Laser Treatment for Macular Edema more than once to control the leaking fluid. If you have Macular Edema in both eyes and require laser surgery, generally only one eye will be treated at a time. Laser treatment of Diabetic Macular Edema works to stabilize vision. In fact, Laser Treatment may reduce the risk of vision loss by 50 percent. In most cases, early laser treatment and/or intravitreal injections of Vascular Endothelial Growth (VEGF) Inhibitors such as Lucentis®, Avastin® or Eylea® Injections will reduce the swelling and prevent further vision loss, but may not restore vision that has already been compromised. In a small number of cases, if vision is lost, it may be improved. It is important to restate that this treatment is performed to keep vision form further declining, but does not usually result in improvement in a vision already lost. This is why it is so crucial to have regular eye examinations as the goal is to diagnose vision-threatening disease before vision is compromised.






